Peptide Payload

More than 10 percent of pregnant women develop serious complications during pregnancy. The underlying cause is often a poorly functioning placenta, the organ that nourishes and maintains the fetus.
A new study by an international team of researchers, including UC Santa Barbara’s Erkki Ruoslahti, has found a way to bolster the placenta during pregnancy. The discovery could one day help prevent some premature births and treat complications such as preeclampsia, a condition characterized by high blood pressure and sometimes fluid retention. The findings appear in the journal Science Advances.
“Our findings emphasize the similarities between placentas and tumors,” said co-author Ruoslahti, a distinguished adjunct professor in the Center for Nanomedicine and Department of Molecular, Cellular, and Developmental Biology and at the Sanford Burnham Prebys Medical Discovery Institute in La Jolla. “That similarity makes it possible to take some of the existing tumor-homing peptides and make use of them in targeting drugs to the placenta. This paper shows that it is possible to increase the delivery of drugs into the placenta via these peptides.”
Certain pregnancy complications are the result of the placenta not growing or functioning properly, but currently there are no drugs that can be used to treat them. Instead, doctors have to induce early delivery, which puts the infant at increased risk of developing infections and cerebral palsy in the short term and heart disease and diabetes later in life.
This new research holds potential to avoid these problems by treating the baby in utero, thereby avoiding induced labor. The scientists demonstrated that two peptides — chains of amino acids — originally used to selectively target tumors can perform the same function on a placenta, delivering drugs that improve the organ’s function and benefit the growing baby without causing harm.
“Placentas behave like well-controlled tumors,” said lead author Lynda Harris of the University of Manchester in England. “They grow quickly, produce growth hormones and evade the immune system. A lot of cancer research focuses on finding ways of delivering drugs to kill the tumor without affecting the rest of the body. We had the idea that if we could selectively target the placenta in the same way, we could deliver other drugs to help improve placental function and therefore treat pregnancy complications.”
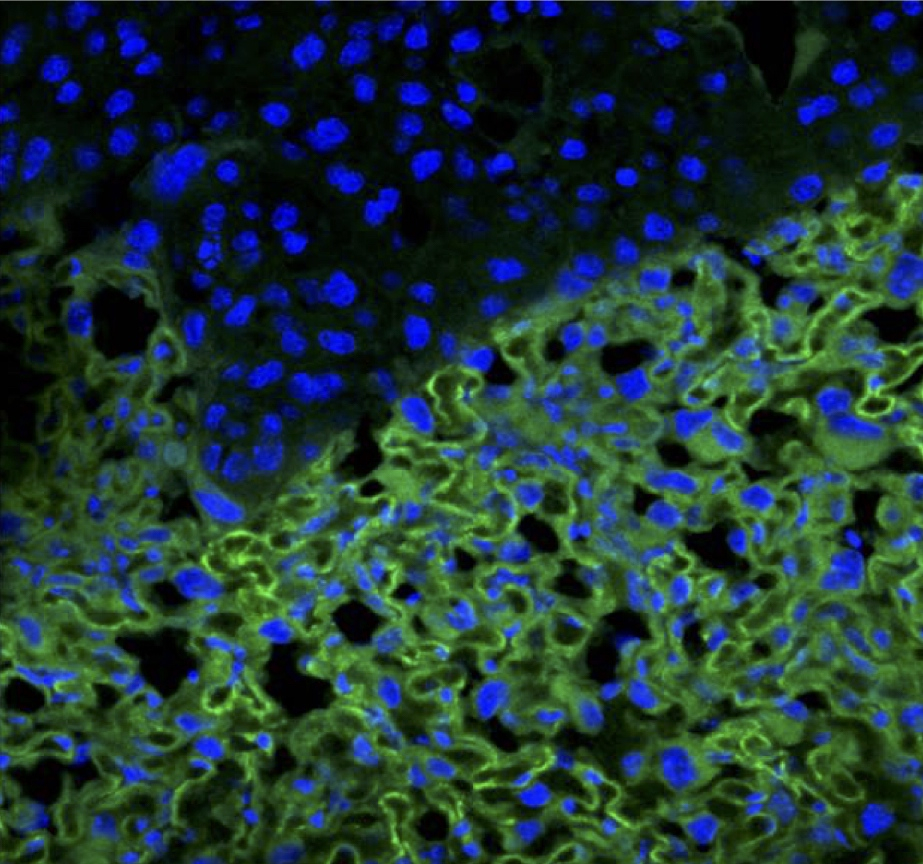
Using a mouse model, the researchers delivered a growth hormone to the placenta via peptide-coated nanoparticles. The drug had no effect on normal-sized fetuses but caused undersized ones to grow.
The targeted drug did not build up in the mother mouse’s organs, nor was any level detected in the fetuses, suggesting that this method has the potential to one day be used in humans. The possibility of potential harmful effects still exists for mothers who have undiagnosed cancers because the drugs also target their tumors, but a screening program could overcome this problem.
“Only one drug for use during pregnancy has been licensed in the last 20 years,” Harris said. “By developing this platform, we have opened up the possibility that any number of new drugs can be adapted and then used safely to treat common and serious pregnancy complications.”



