Bacterial Warfare


It’s bacteria against bacteria, and one of them is going down.
Two UC Santa Barbara graduate students have demonstrated how certain microbes exploit proteins in nearby bacteria to deliver toxins and kill them. The mechanisms behind this bacterial warfare, the researchers suggest, could be harnessed to target pathogenic bacteria. Their findings appear in the Proceedings of the National Academy of Sciences.
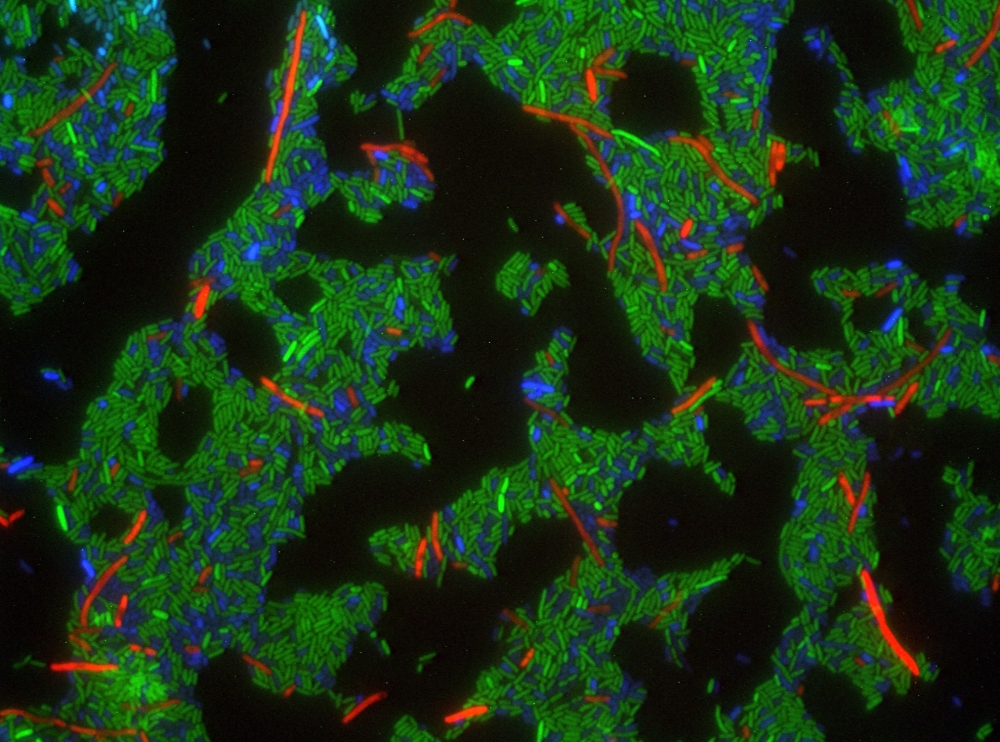
Lead authors Julia L.E. Willett and Grant C. Gucinski have detailed how gram-negative bacteria use contact-dependent growth inhibition (CDI) systems to infiltrate and deliver protein toxins into neighboring cells. By studying the bacteria Escherichia coli (E. coli), they were able to document how CDI “translocation domains” can use multiple pathways to transfer those toxins into a cell. By understanding that mechanism, Willett said, it could be possible to use it as a model for pinpoint targeting of bacteria.
“The long-term, real-world potential is that if we know bacteria can deliver their own proteins into other cells, we might be able to use this as a delivery system for antibiotics and other therapeutics,” said Willett, a doctoral student in UCSB’s Department of Molecular, Cellular and Developmental Biology (MCDB). She and Gucinski conducted the work under the direction of faculty adviser and MCDB professor Chris Hayes. Hayes is the second author on the paper.
“If we know the detailed mechanisms of delivery maybe we can target specific groups of bacteria,” Willett continued. “Instead of taking an antibiotic that targets all bacteria, we might be able to deliver one that could specifically target one group of bad bacteria that leaves the good bacteria in your gut alone.”
Gucinski, a graduate student researcher in UCSB’s Biomolecular Science and Engineering Program, began studying E. coli as an undergraduate. Although it has a reputation as a nasty pathogen, that group of bacteria is generic enough to make an ideal research subject.
“E. coli is the easiest system to work with and very representative of the majority of other bacteria,” Gucinski said. “The kind of CDI systems that we study are also found in a lot of different kinds of bacteria. This is the tip of the iceberg in our understanding of what we’ll find in other CDI systems in other bacteria.”
CDI were first described by David Low, professor of MCDB, in 2005. Low, a co-author of the current PNAS paper, reported how a bacterial cell would touch a neighboring cell — one that was competing for resources in the environment — and inject it with a toxin. Willett and Gucinski’s research builds on Low’s work by identifying the multiple ways CDI toxins exploit target cells. The key was in understanding the genetics of those targeted bacteria.
“We know that the cells would have these CDI systems; we know the genetics that are required to make this toxin system, but we were interested in the genetics on the other side, the genetics that are required in the cell that’s being inhibited or the cell that’s receiving this toxin,” Willett explained. “What specifically in that cell is required for the toxin to go from outside the cell to inside the cell?”
Willett and Gucinski found that mutations in the target cells allowed CDI to exploit those cells and inject them with toxins.
“What these CDI systems have done is they’ve actually hijacked machinery that the cells already have,” Willett said. “And so cells when they’re growing need to take in nutrients, and the CDI systems hijack those pre-existing systems to deliver these toxins. It’s not really tricking the target cells, but it’s basically hijacking what’s already there for the inhibitor cell’s own benefit.”
Looking ahead, Willett and Gucinski say potential therapeutic applications are tantalizing but years away. “We’re still trying to understand the routes that we can get different CDI toxins into the cell,” Gucinski said. “One interesting direction would be what other cargo we can deliver with E. coli, how we can manipulate and control the system to target the pathogens.”
Given the rise of drug-resistant bacteria and a dearth of research into new antibiotics, Willett and Gucinski’s research has the potential to open a new front in the fight against pathogenic bacteria.
“We hear on the news that a lot of pathogens are becoming resistant or people can no longer take certain antibiotics,” Willett said. “And so this might be a new way to get around that. Instead of treating everything on a broad spectrum, if we could learn how a natural antibacterial system delivers things that kill other bacteria we might be able to more learn how we can deliver things like specific proteins or specific antibiotics to kill other bacteria.”
Also contributing to the research was UCSB undergraduate Jackson P. Fatheree. The study was supported by a grant from the National Institutes of Health and a National Science Foundation Graduate Research Fellowship.



