Seeing is Believing
Age-related macular degeneration (AMD) is the leading cause of vision loss in the United States among people age 50 and older. It is estimated that 11 million people in the United States have some form of age-related macular degeneration, and the number is expected to double by 2050.
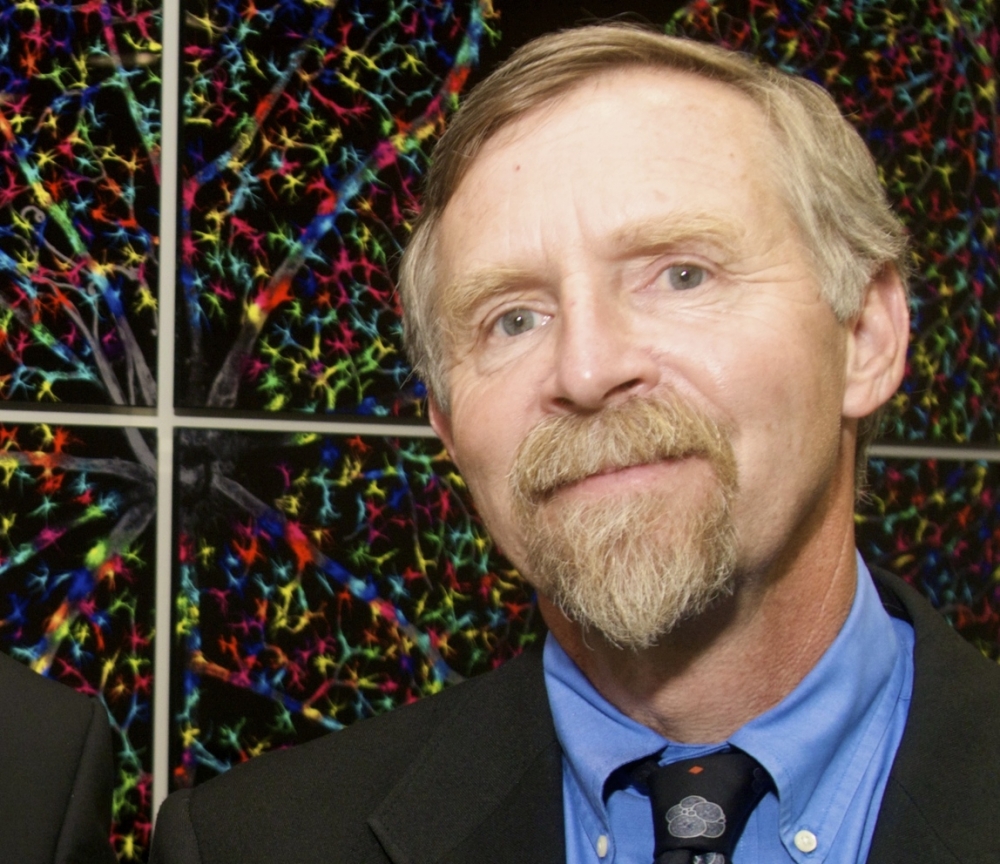
Pioneering research using stem cells to regenerate eye tissue conducted by UC Santa Barbara’s Dennis Clegg and co-workers may one day help people with AMD. As the first person to hold the newly endowed Wilcox Family Chair in BioMedicine, Clegg, a professor in the Department of Molecular, Cellular and Developmental Biology, is poised to bring stem-cell-based therapy for AMD to Phase I clinical trials.
Supported by a generous gift from alumni Sue and Gary Wilcox, the chair is designed to further pre-translational work on human biological systems that may lead to clinical studies.
“I am so grateful to Gary and Sue Wilcox for their generosity in creating the Wilcox Family Chair in BioMedicine,” said Clegg, who is also a co-founder of campus’s Center for Stem Cell Biology and Engineering. “It will help fund innovative, high-risk, high-gain research as well as provide seed money to support students and postdoctoral scholars.”
Clegg is also co-director of the California Project to Cure Blindness, a collaborative effort aimed at developing a stem-cell-based therapy for AMD. The project is funded by the California Institute for Regenerative Medicine (CIRM), the state’s stem cell agency. Partners in the project include the California Institute of Technology (Caltech), the University of Southern California (USC), the City of Hope and University College London.
AMD takes two forms: wet and dry. In the wet form, for which treatment is currently available, growth of abnormal blood vessels causes blood and fluid to leak into the retina, resulting in vision distortion, blind spots and, ultimately, loss of central vision.
The dry form of the disease, which has no treatment and is the focus of Clegg’s research, is caused by the presence of yellow deposits in the eye’s macula. As these deposits grow in size and increase in number, vision is dimmed and distorted. A concomitant thinning of the light-sensitive layer of cells in the macula eventually leads to the death of a cell type called retinal pigmented epithelium (RPE). These are the support cells for the rods and cones — the eyes’ photoreceptors, which allow light to be translated into recognizable images.
“It’s especially devastating because the visual defect occurs in the macula, which is the center of the retina,” Clegg explained. “That part is used for high acuity vision, so people with the disease end up with a big blank spot in the middle of their field of vision. Some reports estimate that more than 30 million people worldwide have this disease, so there is a real unmet medical need for a therapy.”
The project’s goal has been to develop a protocol for replacing dying RPE with new tissue created out of embryonic stem cells. In fact, the eye’s pupil color comes from the RPE, a black pigmented monolayer of cells behind the retina.
“Our part of the project has been to figure out how to make the cells,” Clegg explained. “We took stem cells and worked out a new protocol to create RPE with high efficiency and high purity. We’ve transferred our method to the City of Hope, which has taken over the manufacture, and we’ve already banked enough cells for the Phase I trials slated to begin next year.”
Caltech designed and built the scaffold that holds the RPE. The material had to be permeable and flexible yet strong enough to withstand the rigors of surgical implantation. “Imagine a 3-by-5-millimeter contact-lens-like material coated with a layer of cells, a little patch,” Clegg said. “Instead of putting it on the front of the eye, it is implanted surgically in the back of the eye where the RPE are.”
The surgical implantation technique was developed by Mark Humayun, a professor of ophthalmology, cell and neurobiology, and biomedical engineering at USC’s Keck School of Medicine, USC Eye Institute and Viterbi School of Engineering. Humayun and his team also devised a new tool that allows precise surgical implantation.
“This has really been an interdisciplinary collaboration between engineers, cell biologists and surgeons,” Clegg said. The research team conducted a variety of experiments over four years demonstrating that the cells can restore vision in a rat model of RPE dysfunction. CIRM funding is in place for Phase I clinical trials, which will begin once the project receives Federal Drug Administration approval.
Despite the fact that UC Santa Barbara does not have a medical school, Clegg noted, a plethora of innovative biomedical research takes place here — research that one day may benefit people with all kinds of degenerative eye diseases.
“I had a student who wrote an essay that summed it up perfectly,” Clegg said. “She wrote, ‘Patients are the jet fuel that keeps researchers motivated.’”



