
Seeing Progress


As we get older, many of our body’s processes start slowing down. For instance, a cut on the hand will take longer to heal after middle age than in youth. That said, it still heals.
Unfortunately, this isn’t the case for the cells at the back of the eye, which simply don’t repair much after we pass age 65. This can lead to age-related macular degeneration (AMD), the primary cause of vision loss in older adults. Over 2 million cases were reported in the U.S. in 2010, and the National Eye Institute estimates AMD will affect more than 3.5 million adults in the country by 2030.
Researchers at UC Santa Barbara have overcome a major hurdle in creating a platform to test therapies for this disease, the most common form of which currently has no treatment. The results appear in the journal PLOS ONE.
Our sharpest vision occurs at the center of the retina, in an area called the macula. “This region is packed full of cones, the cells that are necessary for seeing in detail,” said author Pete Coffey, a researcher at UCSB’s Neuroscience Research Institute. “They are the cells that are involved in reading, recognizing faces, the ability to drive, et cetera.”
Just behind them is a layer of retinal pigment epithelial (RPE) cells. These are responsible for maintaining the health of our rods and cones, the eye’s photo receptors. And these are the cells that stop working properly in AMD.
Age-related macular degeneration comes in two forms. Wet AMD occurs when blood vessels infiltrate the retina. There are treatments for this variety, which aim to prevent the growth of blood vessels where they’re not wanted.
However, roughly nine out of ten cases are what scientists call ‘dry AMD,’ which involves progressive degeneration of the macula simply due to the inability of the RPE cells to heal. And while ophthalmologists can identify the disorder’s onset early on, there are currently no treatments for dry AMD.
“Part of the struggle of finding a treatment option is that we’ve not been able to really model the progression of the disease in cell culture or in animals,” said lead author Lindsay Bailey-Steinitz, a doctoral student in the Department of Molecular, Cellular, and Developmental Biology.
Bailey-Steinitz and her collaborators set out with two objectives in mind. The first was to understand what might be going on at the cellular level as the disease progresses. The other was to develop a model that could be used to test therapeutics.
As the RPE cells flounder in their efforts to repair themselves, a hole develops in this layer of the retina that continues to expand. Bailey-Steinitz aimed to recreate this hole in the lab. She cultured RPE cells on a plate with an electrode, then she zapped them. This created a hole very similar to the one that appears in AMD.
However, these were young cells, so they began healing and mending this hole. That’s great for the cells, but not for the team, which was trying to model the disease. So Bailey-Steinitz shocked the cells again. She found that after 10 pulses of electricity over the course of 10 days, the cells were no longer able to effectively repair the damage.
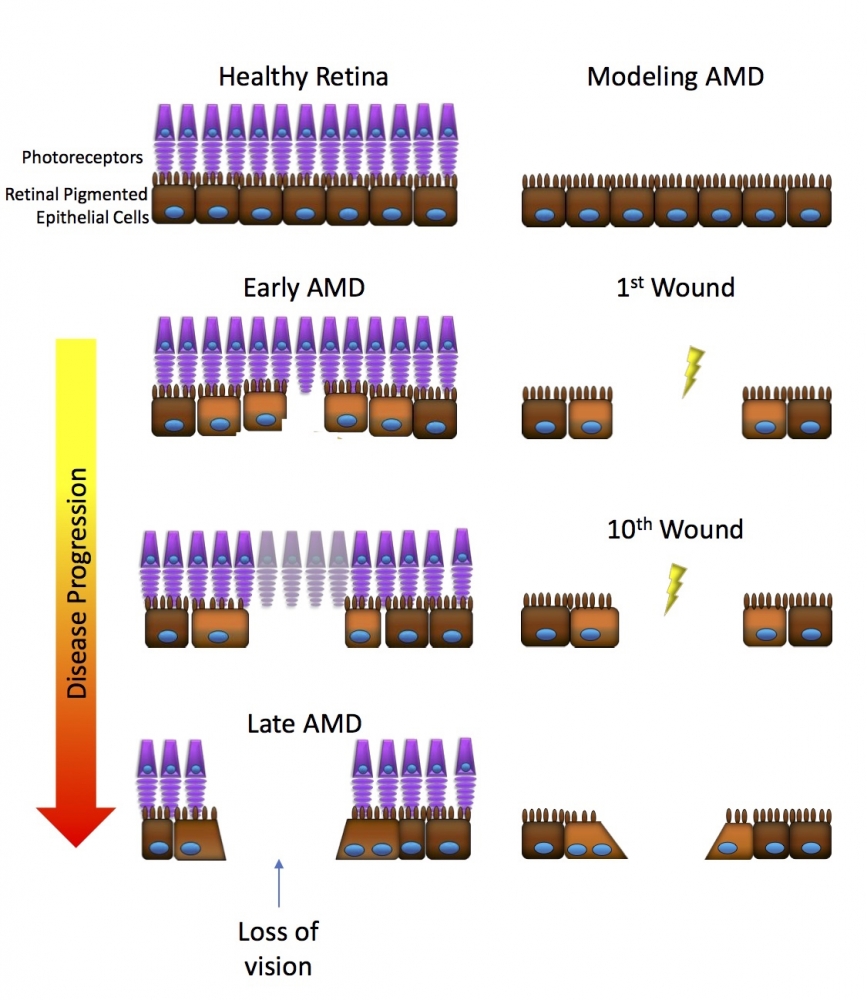
An overview of Coffey and Bailey-Steinitz’s experiment.
Photo Credit: LINDSAY BAILEY-STEINITZ
To shed light on how the RPE cells responded to this stress, Bailey-Steinitz sequenced their RNA to figure out what proteins they were synthesizing in their damaged state. She found that some of the most important genes involved in the RPE cells’ function were suppressed, especially if the cells had been shocked multiple times.
The team also saw changes in gene expression that matched conditions seen in AMD. What’s more, the matrix which provides structural and biochemical support to the RPE cells also changed in ways that resembled the disease pathology.
“I wasn’t surprised that the RPE profile was down-regulated,” Coffey said. “If someone gives you a kick, then you’re not going to feel well.
“But, for that immunology to change — and the matrix around the cells as well — and to look similar to exactly that profile you see in AMD, I was very surprised.”
Now that they’ve recreated a similar profile in cultured cells as in the actual disease, the team is progressing to bigger holes, around six millimeters in diameter. Bailey-Steinitz is also planning a similar experiment with older cells, which show a decreased ability to heal.
“If we can improve this setup, then we’ve got a therapeutic testbed for AMD,” Coffey said.
Funding for this research came from the William K. Bowes Jr. Foundation, Garland Initiative for Vision, and the California Institute for Regenerative Medicine.



